Movember and Menopause
If you’re new to my Substack I’m a two-time prostate cancer survivor that received treatment with drugs that caused side effects that mimic those of perimenopause, menopause and sometimes post menopause. I’m in the unusual position of being a biological man who understands the life challenges that many women experience in their menopause journey. I normally write about menopause with the goal of educating men of how they can support their partner/wife on their menopause journey.
If you’re new to my Substack I’m a two-time prostate cancer survivor that received treatment with drugs that caused side effects that mimic those of perimenopause, menopause and sometimes post menopause. I’m in the unusual position of being a biological man who understands the life challenges that many women experience in their menopause journey. I normally write about menopause with the goal of educating men of how they can support their partner/wife on their menopause journey.
Movember
November is Prostate Cancer Awareness Month so I’m changing up my column and writing about the timing relationship between a woman’s menopause journey and a man’s intersecting risk of developing prostate cancer during that timeframe. Make no mistake. If a man develops prostate cancer while his partner/wife is on her menopause journey, life is going to tougher for both people, at least for a while. Even when prostate cancer is diagnosed as low risk, removal of the prostate and/or radiation to the prostate causes physiological changes that often negatively impacts physical intimacy between partners. It usually doesn’t have to be the end of intimacy but it takes time, patience, and commitment to adjust. When prostate cancer is advanced and aggressive there may be a need for extensive treatment that may interfere with a man’s ability to work and may result in financial hardship for the couple. I’ve seen this happen to friends of mine. The bottom line is that even under the best of circumstances dealing with prostate cancer may present challenges to both partners and if the prostate cancer is advanced and aggressive, the challenges will be even greater. That’s why it’s important to detect cancer when it’s earlier to treat and has a higher likelihood of cure.
My own experience as well as the experience of friends and colleagues has led me to believe that most men have little knowledge of what a woman goes through on her menopause journey. Similarly, most women have a little knowledge of the risk that their partner/husband faces with prostate cancer. Frankly, most men don’t understand what their personalrisk is and what they can do to monitor their prostate health. It’s my hope that since most of my readers are women, my writing will help educate them on the risk that their partner/husband faces and they in turn can educate their partner/husband.
What is the prostate and what does it do?
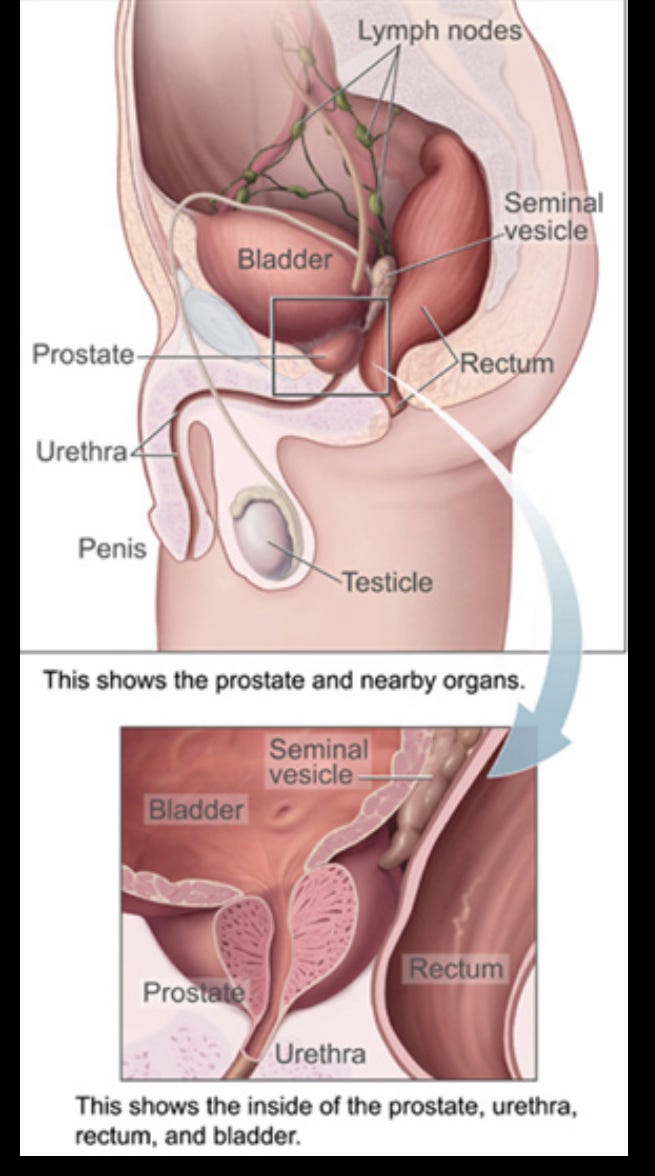
Image courtesy of Wikipedia
The prostate is part of the reproductive system for males. It is a walnut-sized gland that is located between the bladder and the internal end of the penis. Speaking simply, it produces fluid that mixes with semen and provides nourishment to keep sperm cells alive for reproduction. The gland is responsible for ejaculation and rhythmically contracts during orgasm forcing the fluid and semen through the urethra to facilitate fertilization. The prostate also plays an important role in helping a male hold urine.
How do men get screened for prostate cancer?
Screening is done using a simple blood test and optionally, a digital rectal test. The fluid that the prostate produces contains Prostate Specific Antigen, or PSA for short. The blood test is therefore called a PSA test. When the cells of prostate are healthy, very little PSA leaks from the prostate into the bloodstream and the PSA level measures quite low. When the cells of the prostate are unhealthy or damaged, more PSA leaks into the bloodstream and PSA levels measure higher. The presence of cancer in the prostate results in significant cell damage, and the greater the damage, the higher the PSA reading. Most physicians get concerned when the PSA level exceeds 4 nanograms per deciliter in a blood test ( abbreviated 4ng/dLj). A level exceeding 4 ng / dL does not guarantee the presence of prostate cancer, but certainly raises suspicion and concern and warrants further testing. Men 50 years and older should get tested at least once a year for prostate cancer. If a man’s father or brother had prostate cancer, screening should start at age 40.
Some facts on prostate cancer
If you do a Google search you’ll read that prostate cancer affects 1 in 8 men during their lifetime. This statistic is surprisingly nearly identical to the incidence of breast cancer in women. Over the past few years, the diagnosis of prostate cancer has been increasing by 3% a year. It is unclear whether this increase is the result of more men getting screened, an aging population, genetic changes caused by environmental issues, or some combination of all the above. While the average age for a prostate cancer diagnosis is still 68 years, more prostate cancer is being detected in younger men, and 10% of diagnoses are made in men under the age of 55. It’s not necessarily a cause for alarm, but certainly a good reason to start screening at age 50.
Men often act like ostriches and bury their heads in the sand when it comes to facing their risk of developing prostate cancer.
There is a popular myth that getting prostate cancer is almost inevitable and most men will develop it during their lifetime. The myth continues to state that most men will die with prostate cancer present in their body and not even know it. There is no published data to back up this claim. That myth has driven many men to believe that all prostate cancer is slow growing and does not represent a risk that needs to be addressed with regular screening. This leads many men to skip testing and then when prostate cancer is diagnosed, it often is diagnosed in an advanced form that is more difficult to treat and does not have a likelihood of cure.
Prostate cancer that is caught early and treated appropriately has a high likelihood of cure with limited impact on quality of life. Prostate cancer that is caught in later stages often has low rates of cure, but can be often managed with ongoing treatment with varying impacts on quality of life. Prostate cancer is the second leading cause of death for men after lung cancer. Similarly, breast cancer is the second leading cause of death for women after lung cancer. Most women I know start seeing a gynecologist when they enter their reproductive years and undergo annual testing for genital-urinary disease including cancer, and then have annual mammograms starting by age 40. Most men I know only see a doctor when something is clearly wrong or they don’t feel well. Coincidentally, most men I know do not have a Primary Care Physician and do not get an annual physical. An annual PSA test is necessary because prostate cancer is a sneaky little devil. By the time symptoms show up, prostate cancer is typically in an advanced and aggressive metastic form that can be difficult to treat and impossible to cure. Major league baseball legend Ryne Sandberg received an initial diagnosis of advanced and aggressive metastatic prostate cancer in January 2024. I didn’t know Ryne personally, but I’m aware that he was receiving treatment through Northwestern Medicine in Chicago at the same time I was receiving treatment there. As I understand it, “Ryno” was not getting regular screening and so by the time he was diagnosed, he was stage 4 with extensive metastasis. He died about a year and a half later at age 65. His story is not unique. Well over half the men I know that have been diagnosed with prostate cancer we’re not getting screened regularly and when their prostate cancer was found, it was more advanced.
Men that don’t have a designated primary care physician can easily get an annual PSA test without seeing a doctor. I have referred a number of my friends in this situation to Quest labs. One of my female friends made an appointment for her husband, took him out for ice cream and conveniently stopped at Quest Labs to get his blood test done on the way. Bnrilliant! Results are typically available in under a week and presently, as I write this article, the cost for a PSA test is $69. If the lab sees something that’s out of the ordinary or of concern, they typically contact the patient and suggest that they see a doctor for further follow up. Fasting is not necessary, but both sex and bicycle riding should be avoided for at least two days before the test to avoid inaccurate results.
The following is a link to the webpage for Quest health that addresses the PSA test. I have no financial interest and gain no financial benefit from my recommendation of Quest labs as a possible way to get PSA checked what a man does not have a primary care physician. I offer this as a courtesy to save my readers a lookup.
https://www.questhealth.com/product/prostate-screening-psa-5363M.html?utm_campaign=br-mens-health&utm_source=google&utm_medium=cpc&utm_clickid=EAIaIQobChMIvqbWmtrUkAMVHUb_AR1shRcZEAAYASABEgKb8_D_BwE&utm_device=m&utm_keyword=quest diagnostics psa test&utm_content=781736679066&utm_adgroup=prostate&utm_asset=sitelink-prostate&gad_source=1&gad_campaignid=23211037364&gbraid=0AAAAAovgWz7dvpjXCMuF98PF4a4bl70A7&gclid=EAIaIQobChMIvqbWmtrUkAMVHUb_AR1shRcZEAAYASABEgKb8_D_BwE
Don’t let prostate cancer complicate your journey through menopause and beyond. If you have a partner or husband over age 50, make certain he gets screened every year for prostate cancer. You’ll be glad you did.


Love the photo! 😃💝